Ectopic Pregnancy: Diagnosis, Causes, and What to Expect
Understanding Ectopic Pregnancy
An ectopic pregnancy is the establishment and development of the fertilised egg outside the uterus, most often in the fallopian tube. In addition to being an extremely risky pregnancy for the woman, an ectopic pregnancy can cause possibly fatal internal haemorrhage if treatment is not received. It is important to identify this problem early and start treatment to avoid complications that can become life-threatening. In this guide, we’ll delve into the critical aspects of ectopic pregnancy, including its causes, symptoms, and diagnostic process. We’ll also explore what to expect during treatment and address common concerns through a FAQ section. Whether you’re seeking information for yourself or a loved one, understanding ectopic pregnancy can help ensure prompt medical care and better health outcomes.
What is an Ectopic Pregnancy?
An ectopic pregnancy happens when fertilised eggs are typically implanted in the fallopian tube, which is outside the uterus. This, of course, is not a viable pregnancy. The growth of the embryo can be life-threatening to the mother because rupture and internal bleeding are potential complications. A rare condition that occurs in approximately 1-2% of pregnancies, prompt ectopic pregnancy diagnosis is essential. Characteristic symptoms include stabbing pain in the abdomen, abnormal uterine bleeding, and dizziness or syncope. Many women, however, only develop signs when the condition worsens. As such, there’s a need for regular prenatal care. If you suspect an ectopic pregnancy, seek an immediate medical diagnosis to treat it properly.
Ectopic Pregnancy Diagnosis Methods
Medical History and Physical Examination
While the diagnostic steps may commence with presenting symptoms like abdominal pain and irregular bleeding, a thorough medical history and pelvic examination can provide clues to any possible risk factors or signs of ectopic pregnancy and steer further diagnostic procedures to confirm the ectopic pregnancy diagnosis.
Pelvic Ultrasound
The location of the pregnancy is usually found by means of ultrasound, either transvaginal or abdominal. Although a uterine pregnancy secures viability, the failure to find an intrauterine pregnancy with some abnormal findings in the fallopian tube may indicate an ectopic pregnancy.
Blood Tests
The hCG (human chorionic gonadotropin) blood levels are measured. For an ectopic pregnancy, often the hCG will rise slower than expected, and with it, the doctors can assess pregnancy progression and possible viability.
Laparoscopy
A minimally invasive surgical procedure, laparoscopy enables doctors directly to visualise the reproductive organs. It serves not only to determine the location of an ectopic pregnancy but also to outline further treatment procedures.
Culdocentesis
Performed very seldom today, culdocentesis involves introducing a thin needle into the vaginal wall for evidence of blood in the pelvic cavity. This procedure is utilized to diagnose internal bleeding that occurs from a ruptured ectopic pregnancy.
What Causes an Ectopic Pregnancy?
Previous Ectopic Pregnancy
The fallopian tubes may be injured or scarred from a previous ectopic pregnancy, which could make it more difficult for the fertilised egg to travel to the uterine, where it could implant, thereby increasing the likelihood of a future ectopic pregnancy. This is one of the most common causes of ectopic pregnancy.
Inflammation or Infection
Certain conditions, such as pelvic inflammatory disease, which often results from sexually transmitted infections, can lead to the destruction of the fallopian tubes with scarring. Chances for the fertilised egg getting trapped in the fallopian tube are high, leading to an ectopic pregnancy.
Fertility Treatments
Assisted Reproductive Technology (ART) includes IVF, and this increases the chance of ectopic pregnancy. Although IVF assures people of conception, improper implantation is also one of the causes of ectopic pregnancy since the embryo might result in implantation in the fallopian tubes instead of the uterine cavity, thereby increasing the risk of an ectopic pregnancy.
Tubal Surgery
Past tubal surgeries, like tubal ligation or the removal of a fallopian tube, could lead to scarring or changes in the shape and structure. These changes could hinder the movement of the fertilised egg to the uterus and make an ectopic pregnancy more likely.
Contraceptive Methods
Although very uncommon, also at risk for ectopic pregnancy are contraceptive devices like IUDs or failed sterilisation. If a woman does get pregnant, the fertilised egg may not be implanted in the uterus but into the fallopian tube because the fertilised egg cannot pass through the blocked or altered reproductive pathways.
Smoking
Smoking habits causes damage to the fallopian tubes, reducing their ability to transport the fertilised egg to the uterus. The chances of getting an ectopic pregnancy increase with the likelihood that the egg gets stuck in the fallopian tube.
Structural Abnormalities
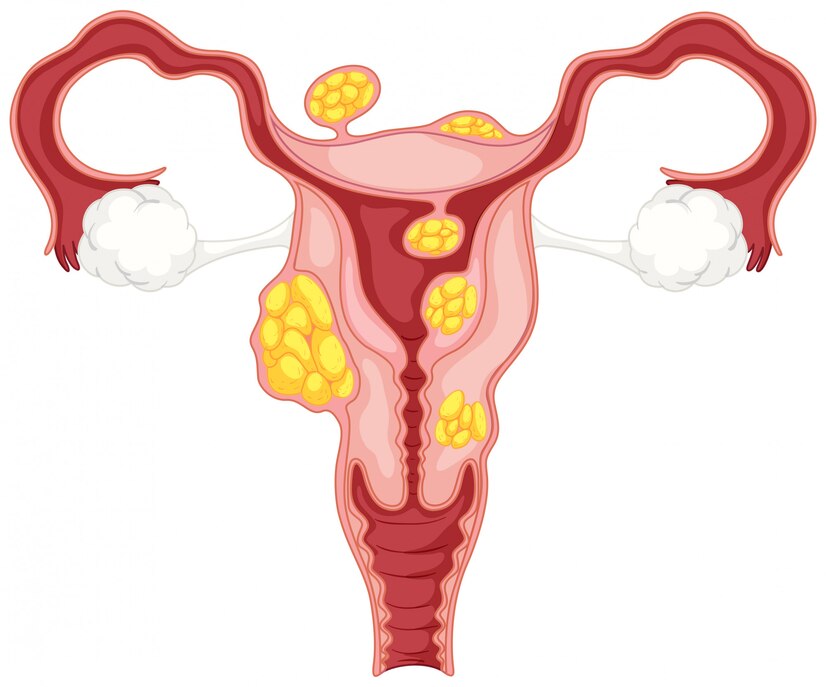
Infertility caused by congenital or acquired structural abnormalities in the reproductive organs, like obstructed or misshapen fallopian tubes, prevents the fertilised egg from properly moving into the uterine cavity. This condition predisposes to the egg possibly being implanted in the fallopian tube, causing an ectopic pregnancy.
What to Expect After Ectopic Pregnancy Diagnosis
After an ectopic pregnancy is diagnosed, the immediate treatment may require administering medication such as methotrexate to prevent the growth of the pregnancy or surgery to remove the embryo. Physically, you will be in pain and tired, but most women recover within a few weeks. Emotionally, this situation can prove to be sad, guilt-ridden, or anxiety-ridden, so support of the psychological kind is crucial in the immediate aftermath. Future pregnancies are monitored through regular check-ups and early ultrasound scans to diagnose possible complications. Waiting before getting pregnant again, as the health provider instructs, is also important so that one can fully recover and the chance of risk factors becomes lower.
Early Action, Positive Outcomes
Ectopic pregnancy diagnosis if conducted early and treated, can avert severe health threats and complications. When one experiences abdominal aches, irregular bleeding, or dizziness, it is important to seek the services of a professional doctor. Factors that predispose you to this condition include a history of having had previous ectopic pregnancies and pelvic infections, as well as fertility treatments. With proper care and treatment, recovery is possible, and many women go on to have healthy pregnancies in the future. Emotional and physical support are also key to healing. Don’t hesitate to reach out to your doctor for advice and guidance on your journey to recovery and future fertility.
FAQ’s
Who can become pregnant ectopically?
Individuals at risk who include history of previous ectopic pregnancy, PID, fertility treatments, or smoking.
Can I have a normal pregnancy after an ectopic pregnancy?
Yes, but it would depend on the severity of damage and overall health. Appropriate medical counseling is necessary.
How do I avoid an ectopic pregnancy?
Minimise risk factors like smoking and untreated infections, and discuss prevention with your healthcare provider.